The content of the article
A stomach ulcer is a disease that affects not only the digestive tract. Its destructive effect falls on almost all body systems. The cardiovascular and nervous systems suffer, a person experiences pain, general health is disturbed. High risk of perforation of ulcers and bleeding, which becomes a threat to life. Therefore, treatment of peptic ulcer should be carried out under the guidance and supervision of a doctor.
Features of the disease
Since the beginning of the twentieth century, the approach to the treatment of peptic ulcer has changed significantly. Initially, it was assumed that the main factor in its occurrence is nerves. The concepts of “stress” and “shock” ulcers, which explain the disturbance of the stomach after stressful situations, have been introduced into medicine.
The reasons
However, over time, the theory of the exclusively neurological component of the disease was disproved. Risk groups were identified based on observations and studies. Determined that:
- men get an ulcer 4-7 times more often than women;
- the disease is 3 times more common among urban residents than in rural areas.
These data allowed us to conclude that the degree of disease risk depends on a person’s lifestyle. And highlight several main causes of the disease:
- excessive passion for spicy, spicy food;
- food without a regime - rare, dry, in a hurry;
- lack of first courses in the diet;
- alcohol abuse.
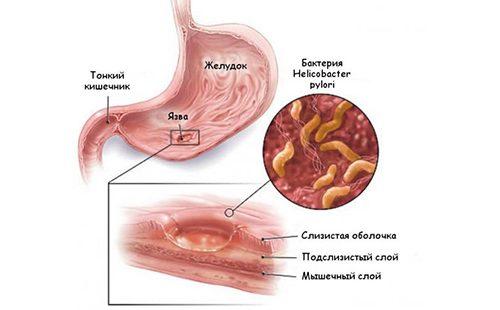
In the eighties of the last century, another reason was identified that causes the development of the disease - bacterial. It was found that in a person’s stomach, with constant exposure to hydrochloric acid, a microorganism can survive that interferes with the normal functioning of the mucous membrane. It is called Helicobacter pylori. Currently, he is assigned the primary role in creating the conditions for the formation of ulcerative lesions of the walls of the stomach.
But Helicobacter pylori is still not the main reason for the development of peptic ulcer. It only supplements a complex of problems, including eating disorders, nervous stress. Its damaging effect on the gastric mucosa can be effectively restrained by local protective factors, in particular mucus. With an increase in the total number of aggressive factors, local defense can no longer cope. There is a local defect in the gastric mucosa, which is exacerbated by exposure to hydrochloric acid, peptins and bile.
Symptoms
The onset of the disease disrupts the gastrointestinal tract as a whole. Often it is accompanied by gastritis, cholecystitis, when the stomach, gall bladder, pancreas are involved in the pathogenic process. The disease causes discomfort and is never asymptomatic.
In the initial stage, the patient may note the following symptoms.
- Pain. Sensations are localized in the stomach and occur regularly.If painful sensations, literally “folding” a person in half, occur after eating, it is likely that damage to the mucous membrane is formed in the stomach. If pain accompanies periods between meals (the so-called "hunger attacks"), this indicates a peptic ulcer of the duodenum.
- Heartburn. It is associated with the release of hydrochloric acid from the stomach into the esophagus, which occurs due to a violation of its digestive function. It may be accompanied by "sour" burping.
- Weight loss. The patient is rapidly losing weight. In combination with other symptoms, this makes it possible to diagnose peptic ulcer with a high probability.
Treatment of ulcers should be carried out exclusively under the supervision of a physician. Modern techniques can normalize the patient's condition and eliminate painful discomfort. The patient is prescribed antibiotic therapy and drugs that accelerate healing, including pantothenic acid, vitamin U.
The role of the correct diet of ulcers
A diet with a bleeding open stomach ulcer is an essential factor for successful recovery. In itself, it does not have a therapeutic effect, as, for example, with gout. But it provides the possibility of effective effects of drugs, reduces the burden on the digestive system, reduces the intensity of the production of hydrochloric acid and relieves pain attacks. If you follow the correct diet during treatment, the patient's condition quickly normalizes.
The principles of therapeutic nutrition
How to eat with a stomach ulcer, without fail, clarifies the attending physician when prescribing therapy. There are uniform principles accepted in international therapeutic practice.
- Follow a sparing diet. Food should not serve as an irritant for the gastric mucosa, therefore it is forbidden to use products with a rough structure, as well as hot and cold dishes. Eat soft, slimy, warm foods.
- Follow table 1. Diet 1 is the recommended standard for peptic ulcer patients. During the period of exacerbation, for ten to fifteen days, stick to "table 1a", which provides for the use of dishes in liquid or jelly-like form. In the future, it is recommended to switch to "table 1b", which corresponds to pureed and gruel-like food. During a period of stable remission, one should be guided by the rules of the standard “diet 1”, which provides for the loose consistency of products, their use in grated or well-ground form.
- Chop food. Puree, jelly-like food not only has enveloping properties and is more easily absorbed by the body. In such a consistency, it does not stimulate the production of hydrochloric acid, which allows the period of exacerbation to be tolerated without severe pain.
- Eat more, move less. A diet with a stomach ulcer during an exacerbation period involves fractional nutrition in small portions. It is recommended to divide the daily ration by at least 5, and preferably 6-7 receptions. At the same time, food should contain a minimum amount of carbohydrates, as they create an additional burden on the stomach and stimulate appetite. The restriction of carbohydrates entails a decrease in the total energy value of the diet, which serves as the basis for the recommendation on the need for patients to bed.
- Include more protein in your diet.. Protein is the building material of our body, and for the effective regeneration of tissues, the body needs it. Eat as many high protein animal foods as possible.
- Do not forget about valuable fats. In particular, about vegetable oil, which should be included in every meal. Unsaturated fats have an inhibitory effect on the secretion of hydrochloric acid, in addition, they themselves are actively involved in tissue regeneration, normalize the cardiovascular system and support the proper functioning of the intestines.
- Reduce salt. It increases the acidity of the stomach, causing discomfort, and increases the recovery period. Use the minimum amount of salt in cooking.
- Add Vitamins to Your Diet. Tissue regeneration necessitates a number of vitamins, which are difficult to obtain from a rather meager diet. Therefore, proper nutrition for stomach ulcers involves taking multivitamin complexes with a high content of ascorbic acid, retinol, riboflavin, and thiamine.
In spring and autumn, special attention should be paid to proper nutrition. In the offseason, the disease, as a rule, recurs, even if complex treatment was previously performed. The correct menu will alleviate unpleasant symptoms or completely avoid relapse.
Compensation of diet in complicated conditions
Diet for gastric ulcer and 12 duodenal ulcer should be adjusted depending on concomitant complicated conditions.
- Vegetative dystonia. Simultaneously with the manifestations of peptic ulcer, symptoms of a violation of the cardiovascular system may occur. In the presence of a heartbeat, changes in blood pressure parameters, frequent sweating, the amount of carbohydrates in the diet should be minimized due to their exciting effect on the nervous system. A good effect is achieved by removing from the diet simple carbohydrates that are quickly absorbed by the body: sugar, sweet desserts, honey.
- Rapid weight loss, slow healing of the ulcer. These conditions may indicate a general depletion of the body, which does not have enough resources for regeneration. It is necessary to enrich the diet with protein food as much as possible, add carbohydrates and vitamins. Unfortunately, a prolonged stay on the diets of the exacerbation period leads to a general weakening of the body - 1a and 1b. Therefore, they should not be adhered to longer than the recommended period.
- Perforation of an ulcer. When a perforated gastric ulcer is formed, the patient needs emergency hospitalization. The heavy bleeding that always accompanies this complication is critically life-threatening. In the first two days, any food is excluded. When the bleeding stops, small meals are allowed, up to two hundred milliliters per day, literally a tablespoon at a time. The diet consists exclusively of cold liquids, in particular milk or cream, liquid jelly. When the condition improves, raw eggs, sour cream, soups with mucous cereals are added to the diet.
- Anemia. It is a consequence of blood loss, so the diet even after minor bleeding should be adjusted. It is recommended that a saturated diet of high energy value, including a large amount of protein food in crushed, mashed form. The amount of fat is limited, while multivitamins and minerals are necessarily introduced, which stimulate the normalization of hematopoiesis. Recommended intake of iron, copper and manganese, ascorbic acid, vitamins of groups B and PP.
- Cholecystitis, liver damage. Involvement of the biliary tract and liver in the destructive process requires a significant correction of the diet. In this case, nutrition with a stomach ulcer during the exacerbation period is determined by the recommendations of treatment table No. 5 (diet number 5) with an increase in the diet of protein foods, a decrease in the level of fat intake and the supply of simple carbohydrates to the body, necessary for the restoration of liver cells and glycogen stores. Sources of simple carbohydrates can be simple sugar or honey, low-fat confectionery.
- Intestinal dysfunction. The gastrointestinal tract can respond to ulceration with multiple problems.Often there is a concomitant bowel disorder manifested by constipation or, conversely, diarrhea, intense bloating and flatulence. When complicating bowel movements, it is necessary to include frayed fruits with a laxative effect in the diet, for example, prunes or beets. Diarrhea, bloating are corrected by a decrease in simple carbohydrates in the diet, which feeds pathogenic microflora.
In this case, the patient should carefully and sensitively listen to his feelings, monitor the digestive tract, regularly consult with a specialist about any changes. Correction of the diet and adapting it to the needs of the patient at a particular point in time can significantly improve the condition, reduce discomfort, and accelerate recovery.

The choice of products for diet
“The most important principle for treating the disease is to protect the digestive system,” comments dietitian Lyudmila Denisenko. “Therefore, the choice of products must be approached reasonably.”
Standard food
During the period of treatment and remission, products that have an irritating effect on the stomach and digestive tract as a whole are excluded.
| Types of dishes | Products |
|---|---|
| Coarse fiber-rich vegetables and fruits | Cucumbers, cabbage, gooseberries, dates |
| Products of animal origin with pronounced connective tissue | Veal meat, cartilage, poultry and fish skin, lard |
| Products stimulating the production of gastric juice spices | Pickles, smoked meats, marinades, fruit and vegetable juices, broths, broths from meat, mushrooms, fish |
| The drinks | Carbonated drinks, coffee, cocoa |
| Spice | Mustard, horseradish, pepper, vinegar, other hot and sour seasonings |
These products should be excluded from the menu for every day for a period of at least four months after exacerbation. Their use is not allowed for two to four weeks in spring and autumn, with the onset of periods of recurrence of the disease.
Products and dishes that the diet allows should be consumed in a warm form, chopped or mashed, pureed. What to eat recommendations include the following products.
| Types of dishes | Features |
|---|---|
| Soups | Vegetarian, on potato or carrot broth; dairy with the addition of boiled cereals (rice, hercules, semolina); dairy with pasta; mashed soups with mashed vegetables, the addition of separately boiled lean meat |
| Bakery products | Dried wheat bread or yesterday’s pastries; dry cookies, biscuit; buns are not edible; baked pastries stuffed with apples, boiled meat or fish, fruit jam; cottage cheese cheesecakes |
| Meat dishes | Steam, boiled dishes of beef, lamb, low-fat pork, chicken, turkey; boiled veal, chicken, rabbit |
| Fish dishes | Boiled fish with low-fat varieties by piece; baked skinless fish steak; steamed fish cakes |
| Milk products | Milk, cream, non-acidic kefir, yogurt, fresh cottage cheese, low fat sour cream, baked cheesecakes, lazy dumplings, puddings, mild cheese |
| Eggs | Raw, scrambled eggs, boiled soft-boiled |
| Cereals | Semolina, round rice, buckwheat, oat |
| Vegetables | Boiled and mashed vegetables, including: potatoes, carrots, cauliflower, beets, green peas, early pumpkin, early zucchini, sweet tomatoes, dill |
| Dessert | Baked, boiled berries and fruits; fruit and berry purees, mousses, jellies; cream cream; milk jelly; honey; jam without sourness; marshmallows |
From drinks choose:
- weak tea;
- herbal tea;
- rosehip broth;
- tea or coffee with milk.

Menu
We offer a weekly menu and diet recipes for stomach ulcers.
| Day of the week | Eating | Food & Dishes |
|---|---|---|
| Monday | Breakfast | Milk rice porridge; rosehip broth |
| Lunch | Soft-boiled egg; toasted bread and butter toast; dried fruits compote |
|
| Dinner | Mashed potatoes; boiled pike perch fillet |
|
| Lunch | Biscuit; tea with milk |
|
| Dinner | Curd pudding; milk |
|
| Tuesday | Breakfast | Lazy Dumplings; weak coffee with milk |
| Lunch | Fruit jelly; biscuit cookies |
|
| Dinner | Mashed oatmeal porridge; boiled rabbit fillet |
|
| Lunch | Tea with milk; marshmallows |
|
| Dinner | Vermicelli with grated cheese; rosehip broth |
|
| Wednesday | Breakfast | Semolina porridge with jam; rosehip broth |
| Lunch | Dried bread toast with butter and low-fat cheese; herbal tea |
|
| Dinner | Combined vegetable puree of potatoes, carrots and cauliflower; steam chicken cutlet |
|
| Lunch | Baked apple with honey; compote of fresh fruits and berries |
|
| Dinner | Steam omelet from two eggs; milk |
|
| Thursday | Breakfast | Low-fat cottage cheese enriched with calcium; Wheat bread toast with butter |
| Lunch | Banana and baked apple fruit puree | |
| Dinner | Rice soup with vegetable broth; boiled chicken fillet; wheat bread toast with butter |
|
| Lunch | Chicken fillet paste with carrots; jelly fruit |
|
| Dinner | Milk soup with vermicelli; herbal tea |
|
| Friday | Breakfast | Buckwheat porridge with milk; rosehip broth |
| Lunch | Cottage cheese with the addition of baked apple; milk |
|
| Dinner | Potato soup with dill; baked perch or cod steak |
|
| Lunch | Fruit pastille; compote |
|
| Dinner | Milk oatmeal porridge with sugar; herbal tea |
|
| Saturday | Breakfast | Steam omelet from two eggs; wheat bread toast with butter and low-fat cheese |
| Lunch | Cottage cheese casserole; milk |
|
| Dinner | Vegetable soup with vegetarian broth; crackers |
|
| Lunch | Kissel fruit; biscuit |
|
| Dinner | Steam fish cutlets; Tea with milk |
|
| Sunday | Breakfast | Oatmeal porridge mucous; soft-boiled egg; wheat bread toast with butter and low-fat cheese |
| Lunch | Meat puree; dried bread |
|
| Dinner | Rice porridge with butter; squash Cavier |
|
| Lunch | Wheat bread toast with butter and low-fat cheese; tea with milk |
|
| Dinner | Lazy Dumplings; sour cream |
The menu is recommended for the period of diet at the remission stage. With a satisfactory condition and a successful recovery, it is allowed to include soft, sweet fruits, as well as tomatoes in general, in the diet.
After operation
Nutrition for gastric ulcer and duodenal ulcer after surgery is prescribed by the attending physician. The standard recommendation is to observe hunger for up to two days with the goal of initial healing of the sutures. Further adhere to the following requirements.
- On the third day. The patient can eat in accordance with diet 0a, provided that he does not have bloating. Fractional nutrition, up to seven times a day. The consistency of dishes is exclusively liquid or in the form of jelly. The first meal should be the smallest, in the amount of one teaspoon. In this amount, the patient is offered hourly juice, diluted with water, fruit jelly, and weak meat broth hourly. Within two days, the volume of a single dose is increased and the patient is transferred to six to seven meals a day.
- On the sixth day. Gradual expansion of the diet and bringing it to the standard diet of table No. 1 by introducing mashed cereals, mucous soups, soft-boiled eggs or in the form of a steam omelet.
The diet should contain the maximum amount of protein components and vitamins, while carbohydrates, especially simple ones, should be minimized. This will saturate the diet with a spectrum of useful substances necessary for a patient with a small amount of servings.
Diet for gastric ulcer performs an important therapeutic function.It determines the success of the treatment of the disease, so you should strictly adhere to its recommendations. Sparing nutrition reduces the intensity of the production of gastric juice, stimulates tissue regeneration, reduces pain and discomfort. The correct diet is necessary until the treatment is successfully completed.

